Patient timeline representation to model EHR data.
Authors
Parth Tandel, Priya Singh, Monica Mishra
Summary
The large volume of healthcare records is difficult to use directly given their complicated relational structure with a wide variety of variables, for instance, the timing of a visit to a hospital, services performed during the stay, initial diagnosis by the primary caregiver, lab reports, etc. As the information is scattered across various tables, any machine learning algorithm is forced to utilize only a subset of features from the dataset. The MIMIC-III1 dataset contains tables namely ADMISSIONS (information about patient visits), INPUTEVENTS (readings of health monitor machines), CHARTEVENTS (record of medicines taken by patients), etc. This dataset contains records of adult patients (aged 16 years or above) admitted to critical care units between 2001 and 2012. The dataset is rich in information yet due to the immense size of tables (~50 GB), it cannot be used directly to predict the length of stay or the readmission chance of a patient. The proposed solution to this problem is the creation of a timeline of events for a patient. The sequence of events captures an exhaustive list of relevant occurrences. Our efforts are heavily inclined towards creating a single source dataset that captures entire information of a patient which advertently makes training an ML model. Based on our study of related previous work2, an important first step to achieve the desired timeline representation is to convert our MIMICIII into a standard format - Fast Healthcare Interoperability (FHIR)3.
This converted dataset in FHIR format would then be transformed into a sequence of events to represent the patient timeline. This created timeline would then be utilized as an input to deep neural network models such as CNN, LSTM. The timeline representation would be effective to build supervised prediction or classification models. Once the data transformed into the desired format we intend to explore the answers for the following questions:
- Predict the readmission chance of a patient.
- Predict the length of stay of a patient at the hospital.
- Predict the survival chance of a patient given an ailment.
Proposed plan of research
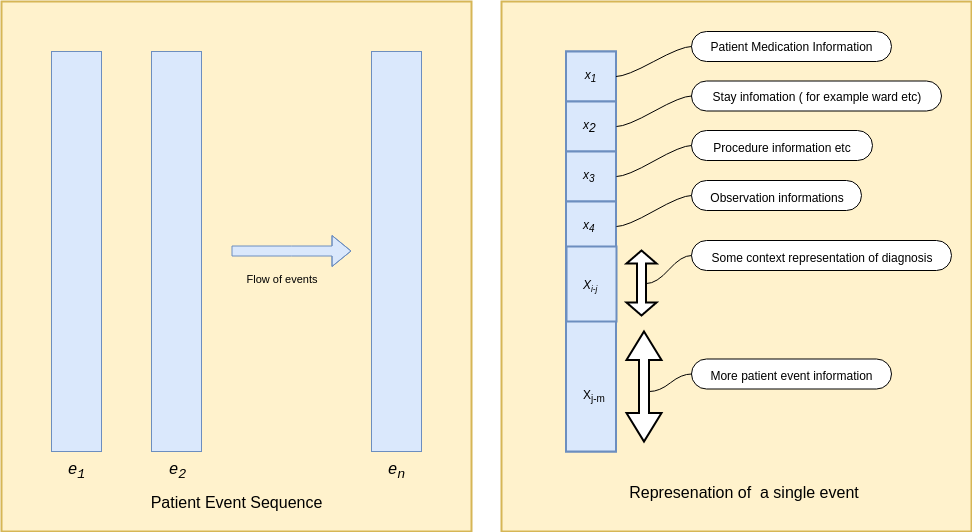
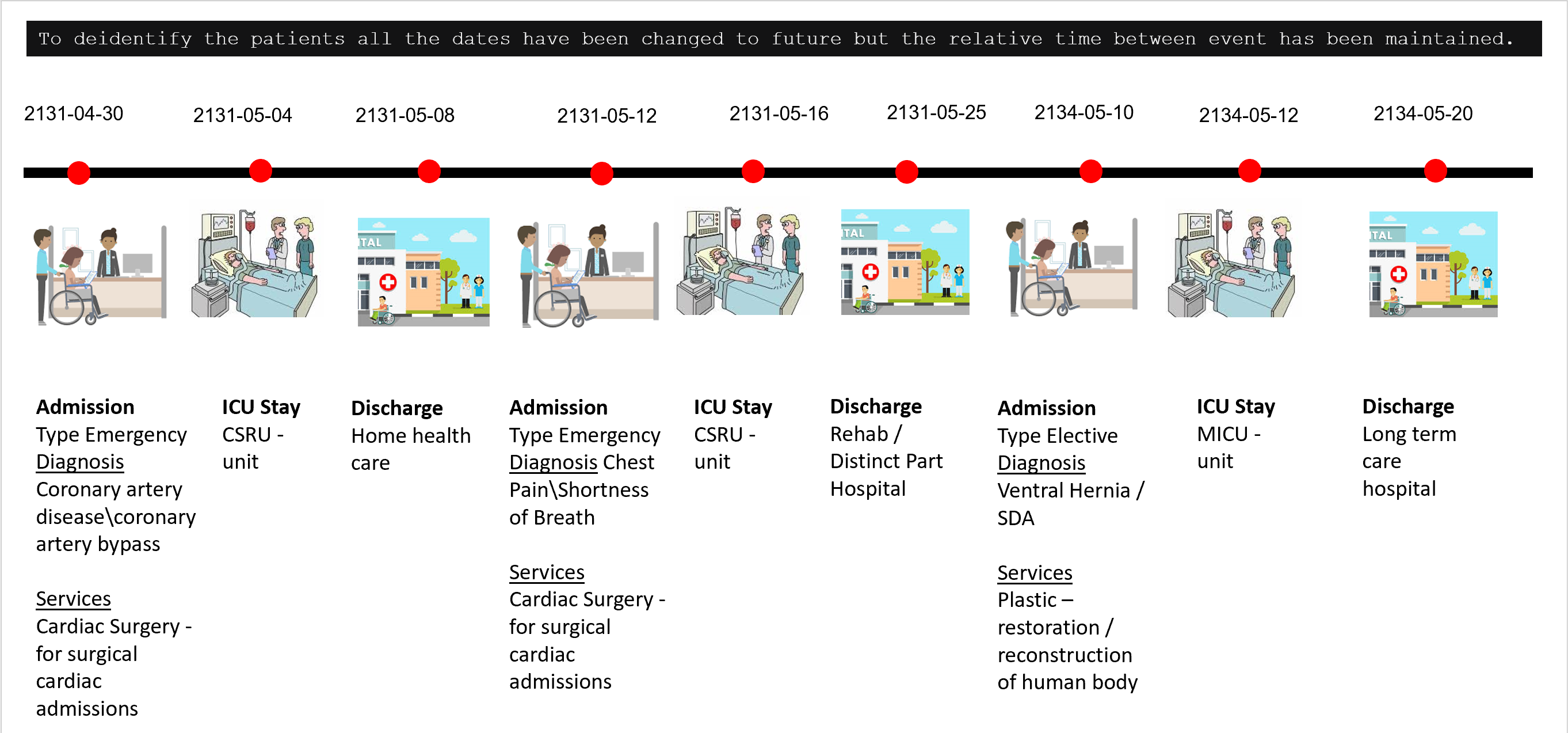
The main task of the project is the creation of a data pipeline to represent a patient's history, after extensive research on restructuring the data, The next phase of the project is to convert the FHIR data obtained from the previous phase to timeline representation and build models on top of it. The first part of this process would be to identify all the feature values required in the sequence. Once these features are identified, they will be extracted. Processing for both numerical values eg. medicine information, chart values, etc and encoding textual information like reports and diagnosis would be done. Using all this information sequence of visits to the hospital would be compiled together. Using this data an LSTM, RNN based model would be trained which would leverage the sequential nature of data and then make a prediction.
Figure 1 : Proposed Timeine represenation of patients Data Figure 2: Patient TimelineWe aim to create sequence vectors to capture the timeline of events using deep neural network techniques such as Long Short Term Memory (LSTM) and Convolutional Neural Network (CNN), and try to answer critical questions for instance:
- What are the chances of a patient to be readmitted?
- How long would a patient stay for a known ailment?
- Is it possible to predict the chance of survival?
Data description
The reason to convert MIMIC to FHIR is that FHIR is a standard next-generation framework created by HL7. FHIR solutions are built from a set of modular components called "Resources". These resources can easily be assembled into working systems that solve real-world clinical and administrative problems. FHIR is suitable for use in a wide variety of contexts – mobile phone apps, cloud communications, EHR-based data sharing, server communication in large institutional healthcare providers, and much more. FHIR data is generally accepted as it is fast and easy to implement. Strong foundation in Web standards: XML, JSON, HTTP, OAuth, etc. makes it a human-readable serialization format that could be easily used by the developers. A challenge faced by healthcare standards is how to manage the diverse variability caused by healthcare processes. As time progresses, many new fields and optional features are getting added that results in additional complexity in managing the base implementation. FHIR tackles this problem by defining a simple framework for extending the existing resources and describing their use with profiles.
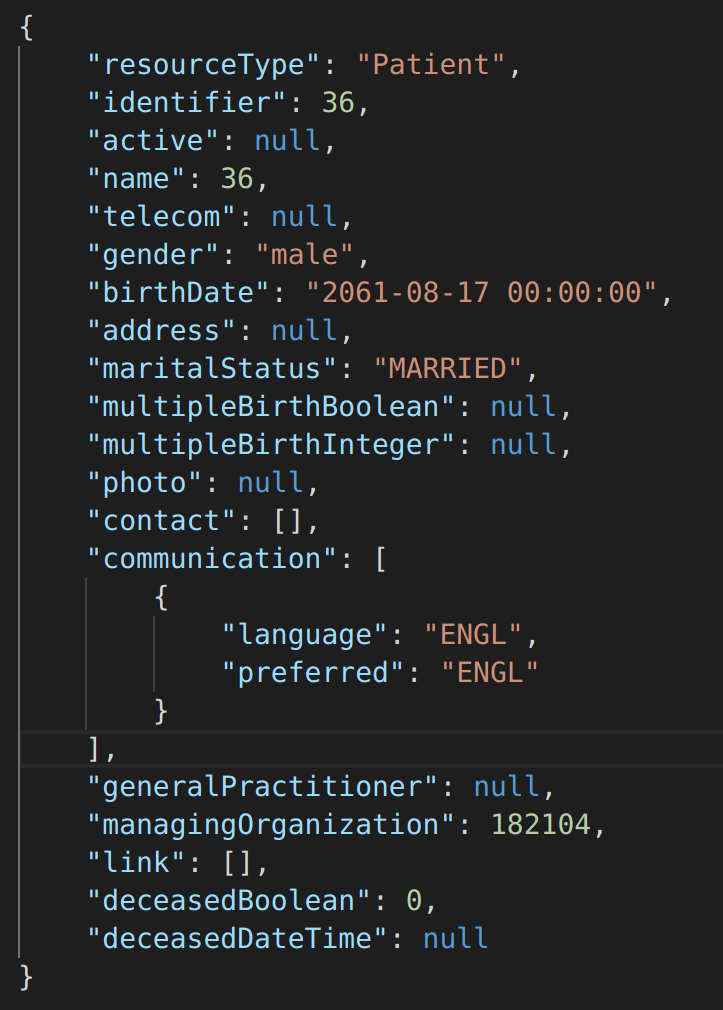
Following are some resources that we selected and converted form MIMIC III dataset:
- Patient resource communicates general information of the patient.
- Encounter resource is about a person’s visit to the hospital.
- Procedure resource has information on the procedures performed on a patient during a single visit to the hospital.
- Report resource discusses the diagnostic reports for a particular patient.
- Medication Dispense resource contains data about the medications given to the patient.
- Observation resource contains lab reports for a patient.
Preliminary results
To get the patient resource in FHIR format as shown in figure 3, the Admission Table and patient table were used to fill out the corresponding information. Similarly, for Encounter resource as seen in figure 4 the information about the patient's visits were found in Admission table, the information about the diagnosis was found Diagnoses_icd and D_icd_diagnoses table, the information about the locations can be found in transfers table and then were compiled together to form Encounters FHIR resource. Similar processes were performed for all other resources.
Figure 3: Patient FHIR Resource Figure 4: Encounter FHIR ResourceReferences
[1] Alpha.physionet.org. (2019). MIMIC-III Clinical Database v1.4. [online] Available at: https://alpha.physionet.org/content/mimiciii /1.4/ [Accessed 28 Sep. 2019].
[2] Rajkomar, A., Oren, E., Chen, K., Dai, A., Hajaj, N., Hardt, M., Liu, P., Liu, X., Marcus, J., Sun, M., Sundberg, P., Yee, H., Zhang, K., Zhang, Y., Flores, G., Duggan, G., Irvine, J., Le, Q., Litsch, K., Mossin, A., Tansuwan, J., Wang, D., Wexler, J., Wilson, J., Ludwig, D., Volchenboum, S., Chou, K., Pearson, M., Madabushi, S., Shah, N., Butte, A., Howell, M., Cui, C., Corrado, G. and Dean, J. (2018). Scalable and accurate deep learning with electronic health records. npj Digital Medicine, 1(1).
[3] Anon, (2019). [online] Available at: https://www.hl7.org/fhir/formats.html [Accessed 5 Nov. 2019].